How to Start Changing Maladapted Shoulder Motion

May 2023 No. 32
How to Start Changing Maladapted Shoulder Motion
by Karol Young, OTD, OTR/L, CHT & Jerry Ditz, DPT, Dip. Osteopractic, Cert. SMT, Cert. DN
Maladaptive Shoulder Movement
A common maladaptive shoulder motor pattern is seen when a patient actively forward flexes the shoulder. To compensate for poor shoulder stability/weakness, patients often also flex the elbow and simultaneously elevate the shoulder when attempting this motion.
Video: Click to watch
When one attempts shoulder forward flexion and the elbow also flexes, the biceps brachii is assisting forward shoulder flexion instead of controlling the humeral head. Current research suggests the long head of the biceps provides glenohumeral stability as well as depression of the humeral head during normal forward shoulder flexion.
When a patient is maximizing arm elevation during shoulder forward flexion, firing the stronger upper trapezius muscle contributes to compensatory scapular rotation. This maladaptive movement pattern leads to shoulder pathology as it decreases the subacromial space, causes pain, and contributes to rotator cuff dysfunction.
Changing the Pattern of Motion
To begin to correct this maladaptive movement pattern, initial treatment should focus on gravity assisted neuromuscular re-education and/or manual cueing.
Gravity Assisted Neuromuscular Re-Education
Begin with active assisted shoulder forward flexion exercises in a supine position to minimize gravity while the patient maintains a corrected posture and uses accurate shoulder movement.
Patient instructions while supine:
1. Grasp a dowel or T-bar with both hands
2. Squeeze shoulder blades together and while maintaining scapular adduction, fully extend both elbows.
3. Forward flex both arms at the shoulder while maintaining full elbow extension. (Figure 1)
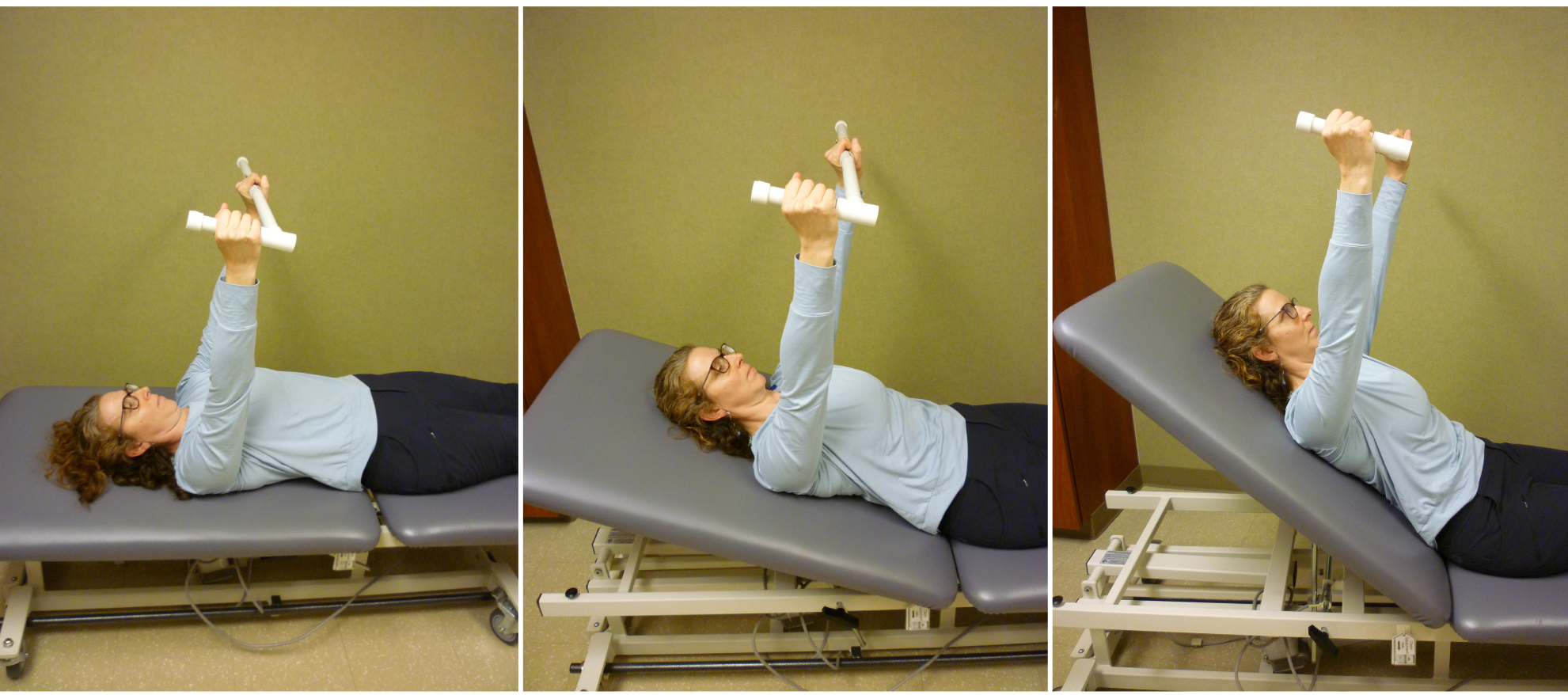
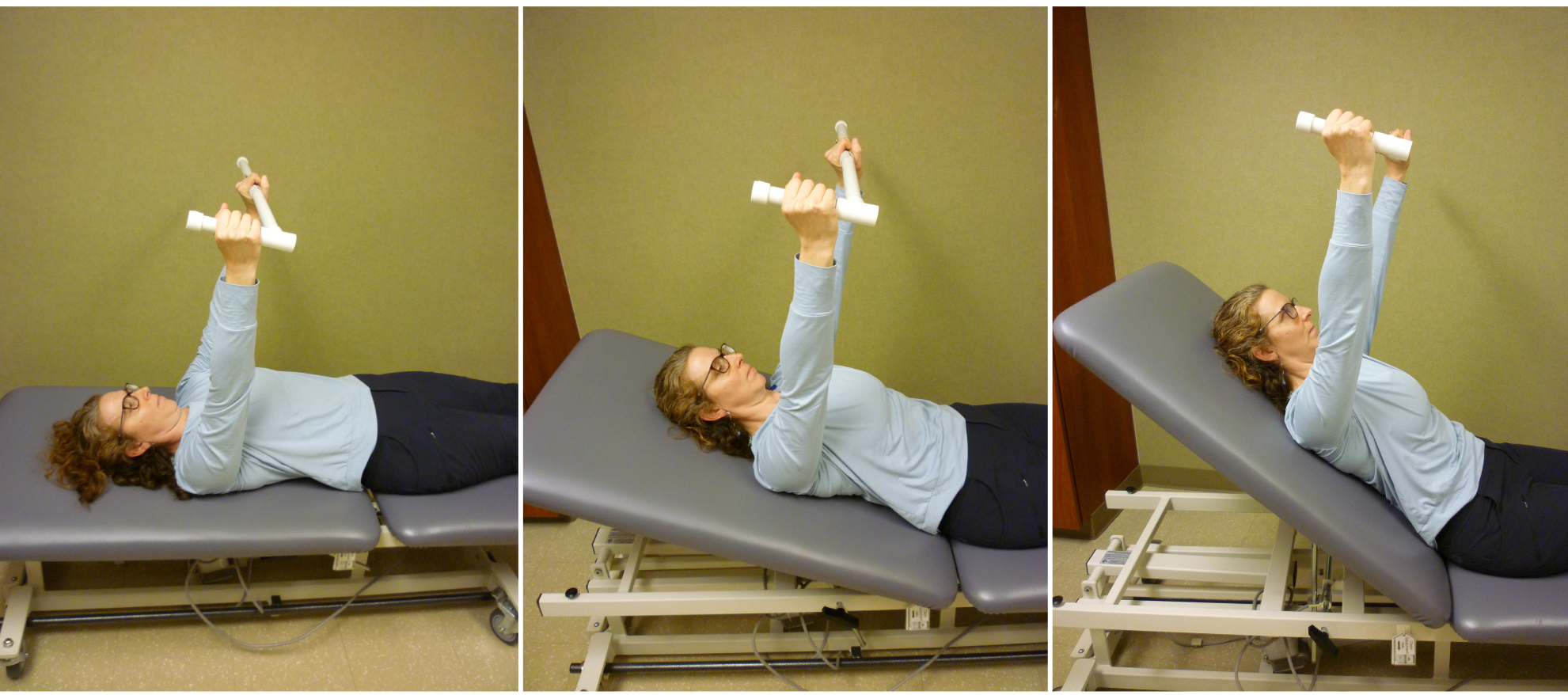
Figure 1: Progression of Active Assisted Shoulder Flexion Against Gravity
Once the patient demonstrates proper technique while supine, progress this exercise by positioning the head of the bed at 45 degrees, and then 60 degrees, and then shift to a sitting position. The slow increase in elevation allows progressive control of shoulder movement against gravity.
When the patient can display these active assistive exercises without accompanying elbow flexion or shoulder elevation, elimination of the dowel or T-bar progresses the exercises to an active exercise against gravity.
The active exercise progression is the same as above (head of the bed at 45 degrees, 60 degrees, and then sitting) (Figure 2).
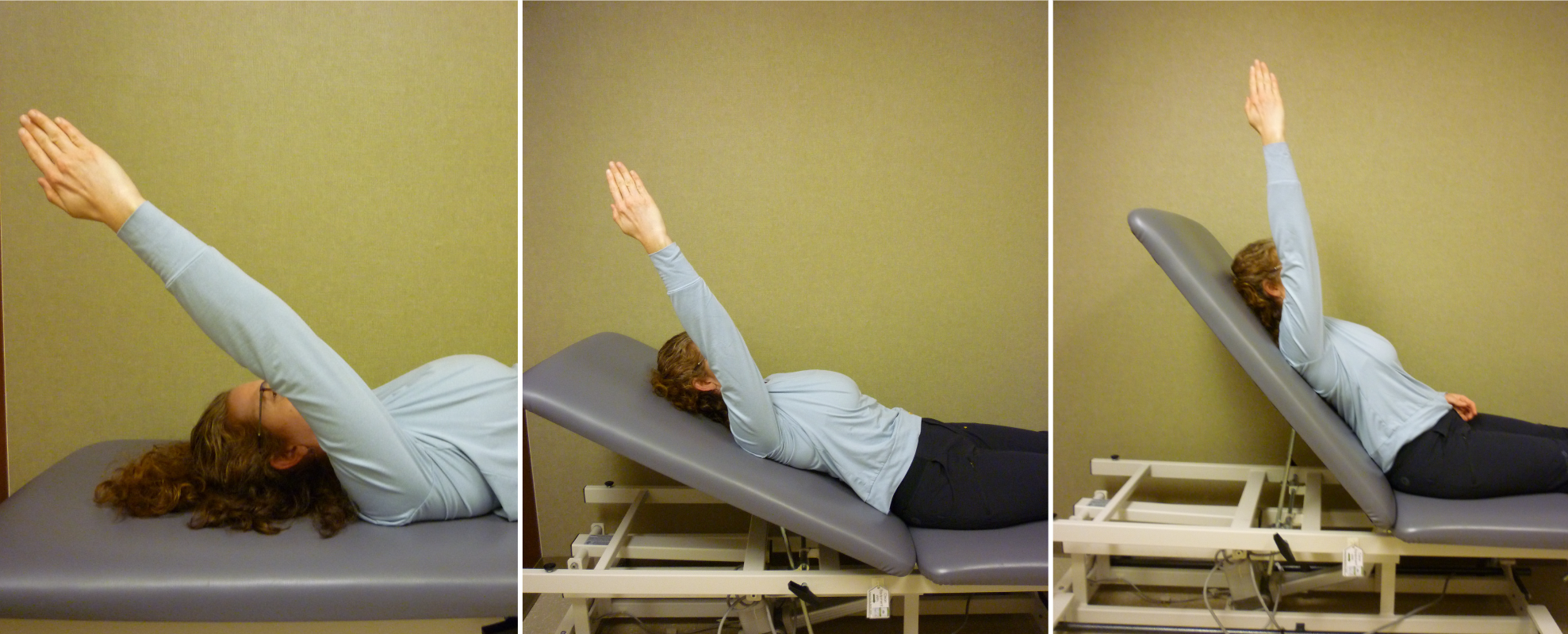
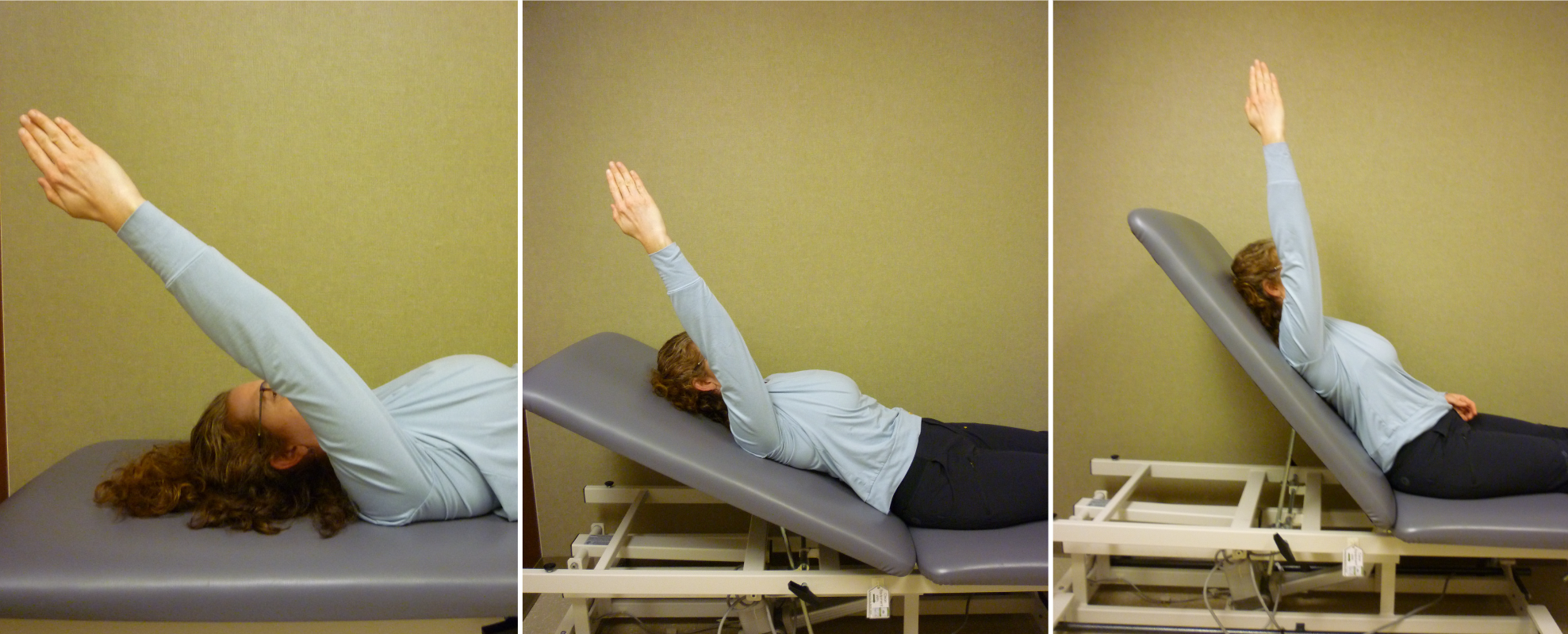
Figure 2: Progression of Active Shoulder Flexion Against Gravity
Gravity Assisted Manual Cueing for Scapulothoracic Control
Because seventeen muscles attach to the scapula, scapulothoracic control exercises improve any shoulder pathology. Manual cueing exercises are often used to improve scapulothoracic control.
Manual cueing exercises focus on decreasing excessive scapular movement and increasing humeral head depression, both of which are needed during the first thirty degrees of active shoulder flexion when the scapula does not normally move so it can act as a stable base for arm movement.
Instructions:
With the patient side lying on the uninvolved shoulder, the affected arm is supported with pillows under the hand and elbow, and the shoulder is positioned in slight abduction and flexion.
Progression I (Scapula Only)
1. Manually position the patient's involved scapula toward slight elevation while the patient resists so the scapula does not elevate; hold between 45 seconds and two minutes (Figure 3).
2. When the patient can no longer maintain the scapular position against your resistance, rest and reposition before repeating.
3. NOTE: It is important to closely monitor scapular and humeral head position to assure the patient is not using maladaptive movements.


Figure 3: Progression I (Scapula Only)
Progression II (Scapula and Elbow)
When the patient can hold the above position for about two minutes, begin to focus on humeral head control by applying force through the humerus to elicit biceps action for humeral head depression:
1. The patient continues to resist manual scapular elevation.
2. Lift the patient's elbow slightly off the pillow while slowly applying manual resistance across the flexed elbow in the direction of humeral head elevation (Figure 4).
3. Ask the patient to resist humeral and scapular elevation between 45 seconds and two minutes.


Figure 4: Progression II (Scapula and Elbow)
Progression III (Entire Upper Extremity)
When the patient can accurately hold the above position for about two minutes, increase the demand required to stabilize the humeral head.
• As the patient continues to resist manual scapular elevation, lift the patient’s arm off the pillow while straightening the elbow and applying pressure though the thumb web space toward humeral head elevation (Figure 5).
• Continue to monitor scapular and humeral position as the patient works to maintain the resistance for two minutes.


Figure 5: Progression III (Entire Upper Extremity)
Once a patient displays the proper neuromuscular firing of the shoulder joint muscles in the side lying position, this same exercise progression is used in a sitting position, and then in a standing position.
Only the Beginning...
The techniques described above are used to begin a comprehensive and progressive treatment program to improve control and create balanced shoulder strength. Changing imbalanced patterns of motion requires accurately focused exercises so all muscles are recruited appropriately. Knowing how to precisely target specific muscles within the shoulder complex establishes the most efficient starting point.
Download Clinical Clue No. 32, How to Start Changing Maladapted Shoulder Motion, May 2023
© BraceLab; 2023 all rights reserved
Disclaimer: BraceLab Clinical Pearls are intended to be an informal sharing of practical clinical ideas; not formal evidence-based conclusions of fact.
