CMMS: How is the Cast Position Determined?

February 2023 No. 77
CMMS: How is the Cast Position Determined?
by Judy Colditz OT/L, CHT, FAOTA & Karol Young, OTD, OTR/L, CHT
Casting Motion to Mobilize Stiffness (CMMS) [go to page 912 in this link] is an effective treatment approach which simultaneously reduces chronic edema and regains limited joint motion while also changing the dysfunctional movement pattern created by the joint stiffness.
One key question when using the CMMS technique is determining the wrist and metacarpophalangeal (MP) joint positions in the cast. The answer comes from observing and understanding normal versus maladapted movement patterns of the wrist/hand.
Wrist Position
A stable wrist is required for the extrinsic flexors to transmit power to the finger joints. A hand without wrist extension, as seen in radial nerve palsy, limits finger flexion because of the passive tension on the opposing extrinsic extensors (See Figure 1).


Figure 1: Limited finger flexion seen in radial palsy
Wrist extension removes the extrinsic extensor tension and allows the extrinsic finger flexors their maximum mechanical advantage (See Figure 2). Excessive wrist extension places tension on the extrinsic flexors, which also dimishes finger flexion power. Therefore, the optimum wrist position is 20 to 30 degrees of extension.
Figure 2: Wrist extension allows maximum finger flexion
For CMMS to alter a maladapted flexion movement pattern, the wrist must first be stabilized in slight extension. If a wrist fracture is the cause of stiffness, one may be reluctant to immobilize the wrist in the cast. But wrist rehabilitation can only occur if the fingers can engage with the environment, making it advisable to focus first on regaining finger motion.
If 20 to 30 degrees of extension is not possible in the first cast, each cast change should serially extend the wrist until this position of wrist extension is reached. When educating the patient on CMMS benefits, manually supporting the wrist in extension while the patient actively flexes the fingers allows them to observe a more normal finger flexion pattern. This enables the patient to understand the need for wrist immobilization.
Many patients with hand stiffness are unable to actively stabilize the wrist when attempting finger flexion, especially if passive wrist extension is also limited. As the wrist is serially extended (if necessary) in the CMMS cast, finger flexion improves. The patient is usually unable to actively extend the wrist before being placed in a cast, but one often observes spontaneous, synergistic active wrist extension with finger flexion upon cast removal! It appears the wrist extensor muscles are activated in the cast.
The wrist extensors, however, are weak, as would be expected. This weakness dictates that cast weaning must begin with only very short periods out of the cast; otherwise wrist extension will quickly fatigue, causing the accurate finger flexion pattern to disintegrate.
MP Joint Position: Regaining IP Joint Flexion
The most common maladapted pattern in the stiff hand is the Dominant Interosseous Flexion Pattern:
• Characterized by starting finger flexion at the MP joints rather than the interphalangeal (IP) joints (See Video)
• Caused by significant interosseous muscle tightness.
• Exacerbated by IP joint stiffness and/or limited flexor tendon glide.
With the wrist stabilized in slight extension in the cast, the MP joints are immobilized in extension, driving all flexor power to the IP joints, with the focus on the pull-through of the flexor digitorum profundus (FDP) muscle (See Figure 3). If any of the three ulnar fingers are stiff, all three finger MP joints should be included in the cast. Be sure the patient always flexes the three ulnar fingers together.
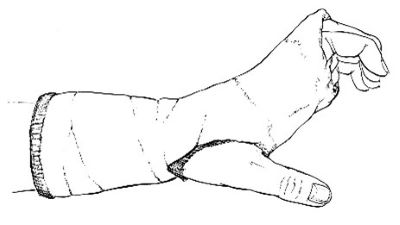
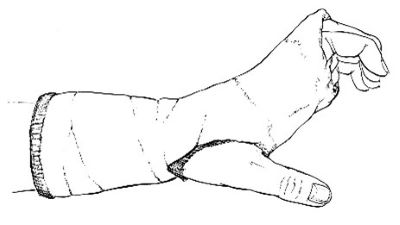
Figure 3: Cast to immobilize the MP joints in extension
Many patients are initially unable to recruit the flexor digitorum profundus muscles, which are needed to drive full IP joint flexion. A dorsal hood can be added to the cast over the IP joints or a small dorsal splint to block the DIP joint into some flexion can be taped to the middle phalanx of each stiff finger. The patient is asked to concentrate on the first motion being the movement of the fingernail away from the dorsal hood/block above it.
Many therapists and surgeons are reluctant to position the MP joints of a stiff hand in extension because we have been taught that the configuration of the MP joint collateral ligaments makes regaining MP joint flexion the priority. Our clinical experience with CMMS shows that MP joint flexion will easily be regained unless there has been direct trauma to the MP joint structures, or the extensor tendons/skin are adherent. The single most effective way to regain FDP excursion and mobilize the IP joints into flexion is to prevent the MP joint flexion.
However, if the patient has stiff IP joints, significant interosseous muscle tightness, edema, and diminished flexor tendon glide, the best starting position is slight flexion of the MP joints (See Figure 4). It is difficult to start regaining IP joint flexion by asking the FDP to pull against all of these limiting factors simultaneously.
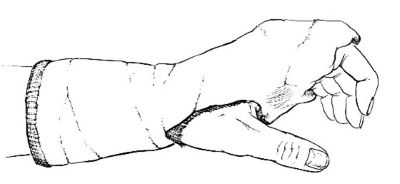
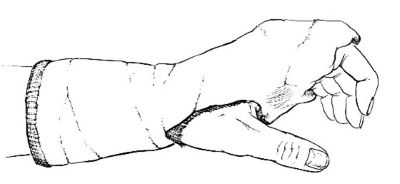
Figure 4: Initial cast immobilizes the MP joints in extension (but not full extension)
Therefore, in some patients the initial focus should first be tendon glide and IP joint motion. When IP joint flexion improves, edema is reduced, and flexor tendon glide within the finger improves, the MP joints should be blocked in full extension so active IP flexion can fully elongate the interosseous muscle tightness. (See Figure 3).
MP Joint Position: Regaining MP Joint Flexion
An injury to the dorsum of the hand often results in adherence of the skin and/or extensor tendons, preventing MP joint flexion but allowing full IP joint flexion. This pattern is a Dominant Extrinsic Flexion Pattern (also called intrinsic minus):
• Characterized by IP joint flexion without accompanying MP joint flexion.
• Caused by MP joint tightness, adherence of the extrinsic extensor tendons/skin on the dorsum of the hand and/or extrinsic extensor muscle tightness.
To regain MP joint flexion, stabilize the wrist in 20-30 degrees of extension in the cast and extend cast distally over the dorsum of the proximal phalanges while holding the MP joints in their maximum easy flexion. On the palmar side, the cast must be proximal to the distal palmar crease to allow full MP joint flexion (See Figure 5).
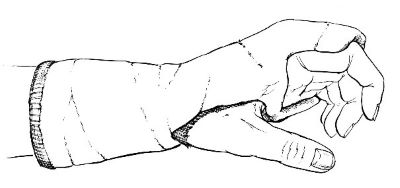
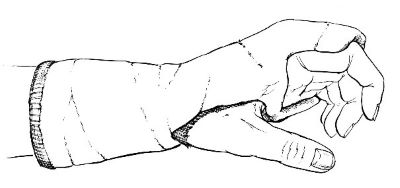
Figure 5: CMMS cast for regaining MP joint flexion
Instruct the patient to pull the proximal phalanx away from the dorsal block with only the PIP joint flexed (superficialis fist) (See Figure 6). Flexing with the “flat fist” demands the interosseous muscles pull the MP joint into flexion. The interosseous muscles are the only primary MP joint flexor; many erroneously attribute this function to the lumbrical muscles.


Figure 6: Active flexion at the MP joints with only the PIP joints also flexed.
The interosseous muscle cannot initiate MP flexion from a neutral position, so some MP joint flexion range must be present before a patient can begin this exercise. It may be necessary to serially position the MP joints until they are in about 20 degrees of flexion. As MP joint flexion improves, the cast is changed, or a pad is inserted between the dorsal hood and the proximal phalanges to hold the MP joints in slightly more flexion.
It is important that the dorsal hood never positions the MP joints in maximum flexion. The MP joints must be allowed to actively flex into the end range, but to return to a less than fully flexed position.
Conclusion
CMMS is a treatment technique that contradicts many things we have been taught about treating the stiff hand, but it is the one effective technique when nothing else works. Observation of your patients’ maladapted motor pattern will direct your choice of wrist and MP joint positions. The thought of casting a stiff hand may feel daunting and counterintuitive, but once you and your patients experience success with CMMS it will become your magic bullet!!
Download Clinical Pearl No. 77, CMMS: How is the Cast Position Determined?, February 2023
© BraceLab; 2023 all rights reserved
Disclaimer: BraceLab Clinical Pearls are intended to be an informal sharing of practical clinical ideas; not formal evidence-based conclusions of fact.
