To Pad, or Not to Pad…That is the Question!

January 2018 No. 48
To Pad, or Not to Pad…That is the Question!
by Judy Colditz OT/L, CHT, FAOTA
Hand therapists frequently need to modify orthoses to relieve pressure of an edge or pressure from an underlying bony prominence. Many therapists add padding. This discussion of a few basic principles may be of value to less experienced clinicians.
Padding Adds Pressure
When padding is added to an area of the orthosis that is already providing too much pressure, the additional padding adds more pressure! Although the padding may dissipate focused pressure (example: sharp edge of orthosis), it does not remove pressure and thus often does not relieve the discomfort.
The solution is to avoid adding padding to the pressure area; instead, add padding around the area of pressure to lift the orthosis off the area.






An easy way to assure accuracy is to mark the location of the pressure point on the patient’s skin with a marker and then quickly apply the orthosis so the ink from the marker transfers to the inside of the orthosis. This mark defines the location around which padding should be added (or perhaps just proximally and/or distally).
There are many different types of padding, a discussion of which is beyond the scope of this Clinical Pearl. Suffice it to say that the padding must not be soft enough that it will compress so it no longer “lifts” the orthosis off the pressure point.
The ideal, however, is to heat the orthotic material and either slightly roll the edge or create a bubble shape over the bony prominence so the orthosis no longer touches the pressure area.
Padding Reduces Stability
The more intimately an orthosis fits the contours of the underlying body part, the greater the ability of the orthosis to stay in place. When padding is added, and especially when excessive padding is added, the orthosis is lifted away from the underlying contour and loses critical stability. For this reason, if padding is used at all it should be the absolute minimal amount necessary. If extensive padding is required for comfort, a new orthosis is likely indicated.
Most Padding is Unhygienic and Difficult to Remove
Adding adhesive backed padding material to the interior of an orthosis is inviting moisture and germs. Removing and replacing adhesive backed padding is often unsuccessful and at best leaves a sticky residue.
If the orthosis cannot be modified to relieve pressure and padding is indicated, the use of removable, washable padding may be the solution.
One method is to affix a narrow sliver of adhesive backed hook on the inside of the orthosis at the desired location of the padding and adhere the padding to the hook. One must use a padding material with a surface compatible with the adhesive hook. Neoprene materials that have a hook compatible side and some soft strapping materials can be used as removable padding.
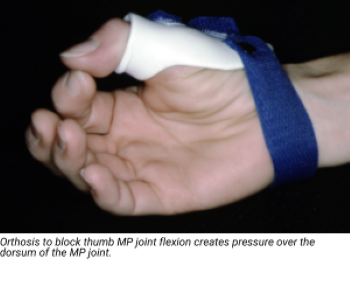
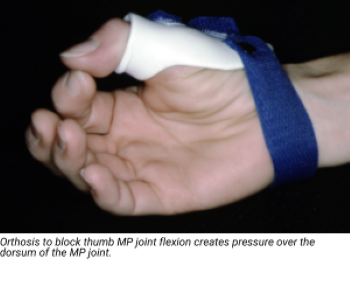
Orthosis to block thumb MP joint flexion creates pressure over the dorsum of the MP joint.


Small neoprene pad is positioned proximal to the MP joint and kept in place with a thin piece of adhesive hook. The pad is removable and washable.
The adhesive hook is kept to the absolute minimum amount to minimize bulk; all that is needed is enough to hold the padding in place. The patient can be given additional replacement pads, and/or the patient can remove, wash, and replace the pads.
Best Solution: No Padding
Of course, the ideal solution is to avoid the need for padding. One suggestion is to identify all potential areas of pressure and raise the contour of these areas before molding the orthosis. One technique is the use of relatively firm exercise putty. (Soft putty will not retain its shape when orthotic material is molded over it.)
Take a small amount of firm putty and roll it into a small ball (or a tube shape, if appropriate). Place the shape over the prominence and gently smooth the putty so there is a soft transition. Place the warm orthotic material over the putty, molding the orthosis. When the orthosis has cooled, remove the putty so there is space between the material and the underlying contour.


Smoothed putty over the distal ulna prominence creates extra space when the orthotic material is molded.
Download Clinical Pearl No. 48, To Pad, or Not to Pad…That is the Question! January 2018
© HandLab; 2018 all rights reserved
Disclaimer: HandLab Clinical Pearls are intended to be an informal sharing of practical clinical ideas; not formal evidence-based conclusions of fact.
